Last review and update: May 6, 2020.
An update: on April 29, 2020, the COVID-19 mortality rate in France reached staggering 18.88%. This is 33 times higher than the COVID-19 mortality in Iceland.
French bureaucrats and medical doctors are criminal morons.


A new gruesome record in France.
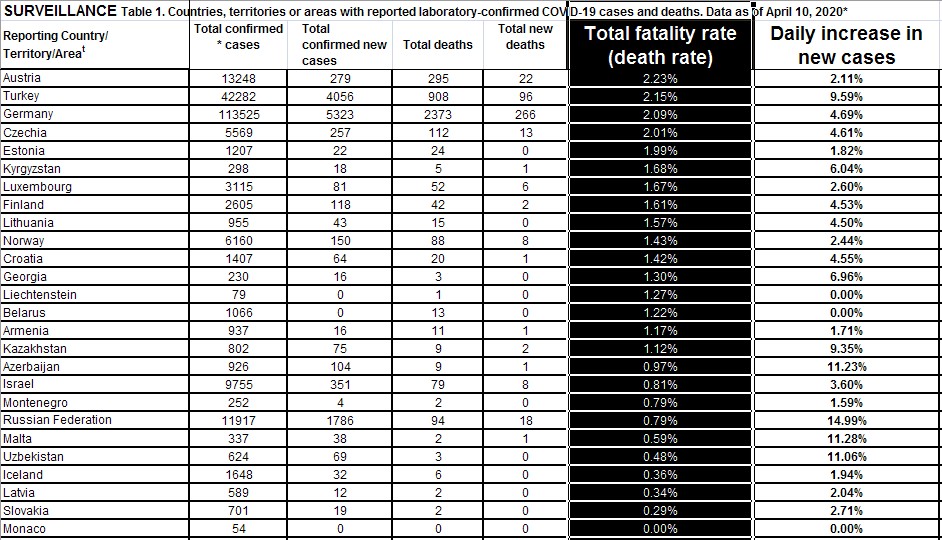
On April 10, 2020, France officially broke a new “record”. The COVID-19 mortality rate in the country reached 14.28%. “Officially” means that this mortality rate is calculated from the data that France reported to the World Health Organization. In the table below, you can see a number of European countries ranked in accordance with their COVID-19 mortality rates as of April 10, 2020.
The Rating of Shame: COVID-19 mortality ranked European countries by the level of incompetence of their medical doctors.

Germany is the most appropriate country for comparison with the European “COVID-19 mortality leaders”. Germany has over one hundred thousand confirmed cases of COVID-19 as of April 10, 2020, and the time between the epidemic onset is comparable with the “COVID-19 mortality leaders”. We can see that COVID-19 mortality rate in Germany remains low, though it is slowly increasing and crossed the barre of 2%. Even 2% is too high.
In a previous article on this website, we argued that the most important and informative statistics would be the COVID-19 mortality rates in each hospital. Then, we can directly compare the competence of the medical teams that work in each hospital.
There is an area in France where the COVID-19 mortality rate is 23% among hospitalized patients.
There is a piece of data that was shared by a medical team from Marseille, France. They are one of the more competent medical teams out there. This piece of data shows different French administrative areas and COVID-19 mortality rates per the total number of hospitalized COVID-19 patients (see below).

What we see in the figure above, is that there is a department in France, an administrative area, where the COVID-19 mortality rate is 23%. Medical doctors in that area treated approximately 7 or 8 hundred patients in hospitals and 23% of them died.
According to the figure, statistically more significant are the data points from the administrative areas where more patients were hospitalized for COVID-19. You can see 2 dots that show two areas where the COVID-19 mortality rate was around 20%. A total of 5 thousand patients were hospitalized with COVID-19 in those to administrative areas.
In some areas of France, between one in five and one in four of hospitalized patients dies.
At this point of time, we can say that in some areas of France, between one in five and one in four of hospitalized patients dies. Such abnormally high mortality rates are horrible. They show abysmal incompetence of the medical teams that work in the hospitals in those administrative areas.
The number of new COVID-19 cases continues to increase by between 4% and 15% a day around the world with only a couple of exceptions.
An update from April 23, 2020: it is more appropriate to calculate the rate of increase in new COVID-19 cases by dividing “the daily new cases” by “the currently active cases”.
We need to note that it is more appropriate to calculate the rate of increase in new COVID-19 cases by dividing “the daily new cases” by “the currently active cases”. As the epidemic continues, more people recover and some die. So, the way the rate of increase in new cases is calculated in the tables below, that is “new cases” divided by “total cases” gives artificially low results as we approach the end of April 2020.
The rate of increase in new cases is an informative piece of data. In the tables below, you can see different countries ranked by the rate of increase in new cases. On average, the number of new cases increases by between 4% and 15% a day. There has not been a significant difference between the countries and areas that are in lockdowns for many weeks and the countries and areas that resisted the “globalist directive” to self-sabotage by shutting down all economic and social life.





“Herd immunity”.
This paragraph required an update since it was first written around April 10, 2020. Indeed, by the end of April 2020, it turned out that only a minority of the population is “susceptible” to get infected with SARS-CoV-2. The curves describing the number of new COVID-19 cases peaked in a majority of countries BEFORE any substantial proportion of the population could get infected.

In this sense, SARS-CoV-2 does not differ from most of the other respiratory viruses. Thus, nobody has immunity for the next year’s influenza viruses. But only a small minority of the population will get infected. The rest of the population is not “susceptible”. Their innate immunes system and their personal hygiene make them resistant to infection. The same applies to SARS-CoV-2.
So, there will be a “herd immunity”, but only “susceptible” will get infected and will become “recovered” and hopefully, “immune”. A majority of the population worldwide will NOT get infected with SARS-CoV-2.


Here is an example to illustrate this. In unvaccinated (against influenza viruses) children from the study by Cowling, 2012 (1), per 1000 person-years, only 88 out of 1412 cases of acute respiratory illness were caused by an influenza virus. That is 6%. We can extrapolate that over 90% of normal unvaccinated children are NOT susceptible to flu viruses.

Medical incompetence.
There is one curve that is really flat during COVID-19. It is the “learning curve” of the medical profession. In 3 months, doctors learned nothing. Mortality is catastrophically high and is increasing.
Medical doctors in Europe and in many other countries tuned out to be abysmally incompetent. A catastrophically large number of COVID-19 patients in their hands die. The large knowledge base available on the very similar SARS-1 (2002-2004) is largely ignored. During the 3 months of the epidemic, the majority of medical doctors learned very little or nothing. There is, thus, one curve that is really flat during COVID-19. It is the “learning curve” of the medical profession.
There are prevention measures that are effective for avoiding getting infected or preventing a severe course of an infection with the SARS-CoV-2 virus. There are also effective “cures”. At this point, avoiding a poor outcome of a probable COVID-19 infection becomes a matter of personal responsibility.
Check if you are prepared to go through COVID-19 epidemics with minimal or no damage to your health and to the health of your loved ones.
Are you ready?
Selected references:
1. Cowling et al., Clinical Infectious Diseases 2012;54(12):1778–83.

2 Comments