Last update and review: October 17, 2020.
A short summary.
In a very recent study, Jhun et al., 2020 (1), the researchers administered a probiotic, Lactobacillus sakei, to mice with collagen-induced arthritis. Collagen-induced arthritis is an animal model that is often used to study rheumatoid arthritis in humans.
What is interesting in this study is that there were measurable the changes of serum IL-17 and IL-10 in the experimental animals. IL-17 and IL-10 moved in the “right directions”.
The interest of these findings for our consulting practice and for medical practitioners in general is that there are biomarkers that we can measure to evaluate the results of our interventions with different probiotics.
Below, there are some citations from Jhun et al., 2020 (1), with more details on their findings and some interesting comments on rheumatoid arthritis and related topics by Jhun et al., 2020 (1), and other authors.
Jhun et al., 2020 (1):
Disruption of normal-flora homeostasis (i.e., dysbiosis) has important immunologic sequalae. In health, the host–microbiome interaction maintains homeostasis. However, dysbiosis has been implicated in several autoimmune diseases [4]. In patients with RA, periodontitis caused by P. gingivalis is reportedly associated with the production of anti-citrullinated protein antibodies [30]; moreover, 16S rRNA sequencing of gut microbiota showed an increased population of Prevotella copri in these patients [18, 31]. Furthermore, P. copri isolated from patients with RA induced the differentiation of Th17 cells [31]. These results indicate a role for the microbiome in the onset of RA. In this study, L. sakei modulated the Th17 and Breg (cells) populations and attenuated arthritis in mice with CIA. Therefore, administration of L. sakei has therapeutic potential for RA.
Administration of Lactobacillus sakei reduced pathologic cytokines in peripheral joints of collagen-induced arthritis animals, the population of Th17 cells and serum level of IL-17, and increased the population of Breg cells and serum level of IL-10.
Jhun et al., 2020 (1):
Proinflammatory cytokines and their source cells are implicated in the pathogenesis of RA; thus, modulation of these cytokines and cells is a target of treatment for RA [20]. Suppression of the inflammatory response with concurrent enhancement of the anti-inflammatory response is the ideal therapeutic approach for patients with autoimmune diseases. Patients with RA have an increased population of Th17 cells and an elevated serum level of IL-17 [32, 33]; modulation of these components has been reported to exert beneficial effects in several animal models of RA [34, 35]. In the context of RA, B cells and plasma cells were previously considered to be limited to the production of autoantibodies, such as anti-rheumatoid factor and anti-citrullinated protein antibodies. However, Bregs also produce anti-inflammatory cytokines and suppress the expansion of pathogenic T cells [25]. In patients with RA, the numbers and activities of IL-10–producing Bregs are reduced, compared to healthy controls [36]. In addition, targeting proinflammatory cytokines, such as TNF-α and IL-6, have shown clinical improvement in RA patients [20], and our results showed decrement of these cytokines in affected joints. In the present study, administration of L. sakei reduced pathologic cytokines in peripheral joints of CIA animal, and the population of Th17 cells and serum level of IL-17, whereas increased the population of Breg cells and serum level of IL-10.
The verdict: Lactobacillus sakei is somewhat exotic, but other commercially available Lactobacilli probiotics could produce similar results.
Lactobacillus sakei is somewhat exotic, but other commercially available Lactobacilli probiotics can be used in addressing rheumatoid arthritis and in other situations where autoimmune or chronic inflammatory processes are suspected.
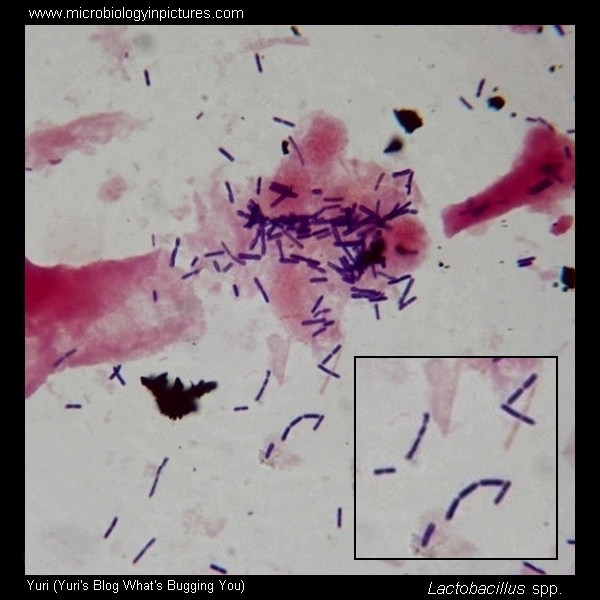
Some info on Lactobacilli, members of the lactic acid bacteria.
Below, there is a citation from Tannock, 2004 (2), that provides a good description of Lactobacilli:
Lactobacilli are members of the lactic acid bacteria, a broadly defined group characterized by the formation of lactic acid as a sole or main end product of carbohydrate metabolism. The lactobacilli are gram-positive, non-spore-forming rods or coccobacilli with a G+C content usually below 50 mol% (22). Eighty species of lactobacilli are recognized at present (55). They are strictly fermentative, aerotolerant or anaerobic, aciduric or acidophilic, and have complex nutritional requirements (carbohydrates, amino acids, peptides, fatty acid esters, salts, nucleic acid derivatives, vitamins). Using glucose as a carbon source, lactobacilli may be either homofermentative (producing more than 85% of fermentative products as lactic acid) or heterofermentative (producing lactic acid, carbon dioxide, ethanol, and/or acetic acid in equimolar amounts). The nutritional requirements of lactobacilli are reflected in their habitats, which are rich in carbohydrate-containing substrates: they are found on plants or material of plant origin, in fermented or spoiled food, or in association with the bodies of animals (22).
Lactobacilli are important in the production of foods that require lactic acid fermentation, notably dairy products (yogurt and cheese), fermented vegetables (olives, pickles, and sauerkraut), fermented meats (salami), and sourdough bread. The use of lactobacilli in the food industry has a long history, and the functions of the bacteria in the industrial setting have been well studied (28). Lactobacilli that inhabit the bodies of animals, however, are much less known, despite an almost continuous interest by scientists spanning about 100 years.

Selected references:
1. Jhun J, Min HK, Ryu J, et al. Lactobacillus sakei suppresses collagen-induced arthritis and modulates the differentiation of T helper 17 cells and regulatory B cells. J Transl Med. 2020;18(1):317. Published 2020 Aug 15. doi:10.1186/s12967-020-02477-8
Below, there are interesting references from the citation above. The numbers are like in the cited extracts.
- Leipe J, Grunke M, Dechant C, Reindl C, Kerzendorf U, Schulze-Koops H, et al. Role of Th17 cells in human autoimmune arthritis. Arthritis Rheum. 2010;62:2876–2885. doi: 10.1002/art.27622. [PubMed] [CrossRef] [Google Scholar]
- van Hamburg JP, Asmawidjaja PS, Davelaar N, Mus AM, Colin EM, Hazes JM, et al. Th17 cells, but not Th1 cells, from patients with early rheumatoid arthritis are potent inducers of matrix metalloproteinases and proinflammatory cytokines upon synovial fibroblast interaction, including autocrine interleukin-17A production. Arthritis Rheum. 2011;63:73–83. doi: 10.1002/art.30093. [PubMed] [CrossRef] [Google Scholar]
- Lee SY, Min HK, Lee SH, Shin HJ, Lee WY, Cho YG, et al. IL-1 receptor antagonist (IL-1Ra)-Fc ameliorate autoimmune arthritis by regulation of the Th17 cells/Treg balance and arthrogenic cytokine activation. Immunol Lett. 2016;172:56–66. doi: 10.1016/j.imlet.2016.02.011. [PubMed] [CrossRef] [Google Scholar]
- Jhun J, Lee SH, Byun JK, Jeong JH, Kim EK, Lee J, et al. Coenzyme Q10 suppresses Th17 cells and osteoclast differentiation and ameliorates experimental autoimmune arthritis mice. Immunol Lett. 2015;166:92–102. doi: 10.1016/j.imlet.2015.05.012. [PubMed] [CrossRef] [Google Scholar]
- Banko Z, Pozsgay J, Szili D, Toth M, Gati T, Nagy G, et al. Induction and differentiation of IL-10-producing regulatory B cells from healthy blood donors and rheumatoid arthritis patients. J Immunol. 2017;198:1512–1520. doi: 10.4049/jimmunol.1600218. [PubMed] [CrossRef] [Google Scholar]
- Kwon MS, Lim SK, Jang JY, Lee J, Park HK, Kim N, et al. Lactobacillus sakei WIKIM30 ameliorates atopic dermatitis-like skin lesions by inducing regulatory T cells and altering gut microbiota structure in mice. Front Immunol. 2018;9:1905. doi: 10.3389/fimmu.2018.01905. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
2. Tannock GW. A special fondness for lactobacilli. Appl Environ Microbiol. 2004;70(6):3189-3194. doi:10.1128/AEM.70.6.3189-3194.2004