The last update and review: July 7, 2022.
Introduction.
The following text is an example of our communications with consulting clients and community members. The names and dates are modified for confidentiality reasons. Parts of the original text are omitted for confidentiality and other reasons. Also, the original text was enhanced with additional information to make this article more informative for the general public.
A message to a community member T.N.
Dear T. N.,
In this communication, we will provide you with information on how to assess vitamin B12 status and on several other points related to your email from January 15, 2022.
A short summary.
The main goal of this communication is to suggest how to assess your vitamin B12 status, to point out the recommended dietary intakes of B12, and to briefly discuss some related topics.
We provide some technical details. There is no need for you to explore them in depth. They can be useful later if you decide to test your vitamin B12 status. Also, they are useful if we want to infer your vitamin B12 status from your past laboratory tests.
We also provide several comments on your answers to our questions from our last email.
What we have learned and inferred from your email from January 15, 2022.
From your email from January 15, 2022, we infer that you are open to consuming dietary carbohydrate.
We believe that being an omnivore is optimal for humans even if humans can adapt to diets with very low or no carbohydrate.
They (some online health personalities followed by T.N. in the past), as most of online health personalities, need to be taken with skepticism and caution. We will discuss the subject later more in details.
We also learned your intakes of added salt. In pre-Columbian Americas, people used to eat without added salt. Humans apparently do not require added salt. However, today, strictly avoiding salt is not always practical.
Your intakes of added salt are apparently low, and your total intake of sodium is likely to be within the “Upper Tolerable Intake” of 2.3g of sodium a day suggested by the Institute of Medicine in the US. Sodium is 40% of salt by weight.
(A reminder: Parts of the original text in this and other sections are omitted for confidentiality and other reasons).
Digestive enzymes sold in pharmacies can be an alternative to the “supplement industry” product that you take as digestive aid.
We have many suggestions about the ways to improve digestion. Dietary interventions are, however, delicate.
You also informed us that you take a supplement to cover your vitamin B12 needs.
The main goal of this communication is to suggest how to assess your vitamin B12 status, to point out the recommended dietary intakes of B12, and to briefly discuss some related topics.
Discussion.
Vitamin B12.
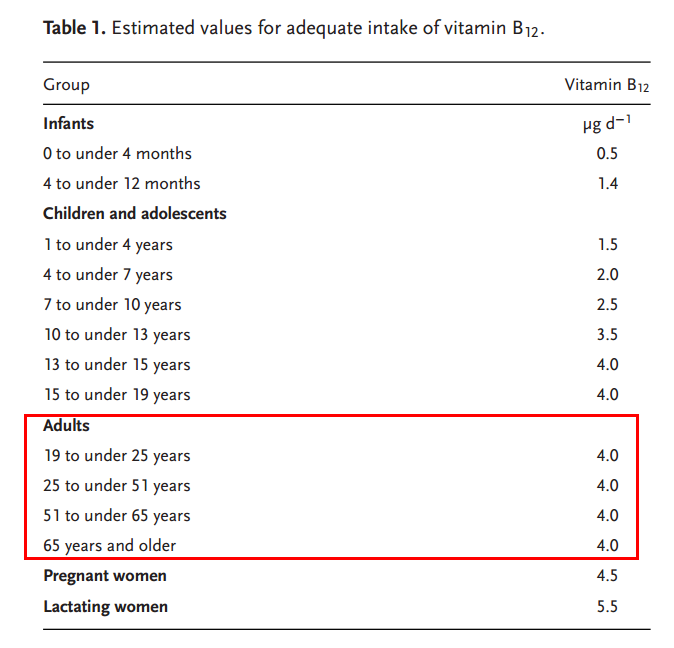
Estimated values for adequate intake of vitamin B12 for Germany, Switzerland, and Austria (updated in 2018).
“Table 4 .Reference values for the intake of vitamin B12 from different nutrition societies.” – Source: Strohle, 2019.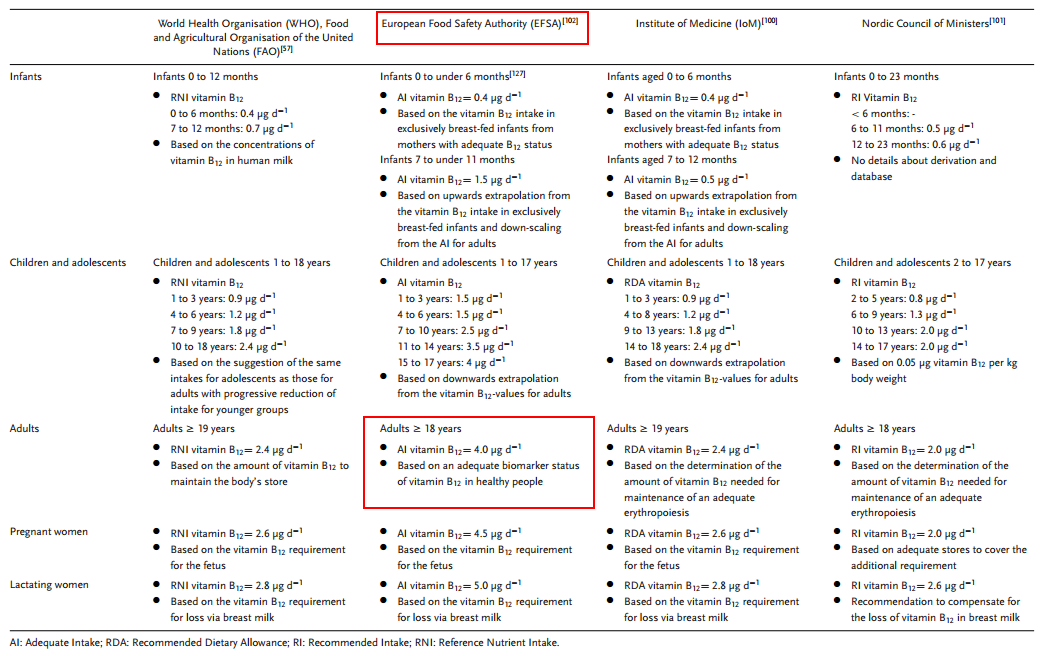 |
To achieve sufficient vitamin B12 intake, a regular intake of animal-based food such as milk and dairy products, fish, poultry and lean meat is recommended.
Strohle, 2019:
“The intake of foods naturally rich in cobalamin as part of a mixed diet can ensure sufficient vitamin B12 supply. To achieve sufficient vitamin B12 intake, a regular intake of animal-based food such as milk and dairy products, fish, poultry and lean meat is recommended.”
Strohle, 2019:
“It should be noted that during food processing, e.g., cooking or pasteurization, a vitamin B12 loss up to 50% might occur.”
Strohle, 2019:
“In older people, the risk of vitamin B12 deficiency is increased, mainly due to impaired absorption because of medication (e.g., proton pump inhibitors, H2 blockers) or diseases (e.g., atrophic gastritis) and less due to insufficient dietary intake of vitamin B12.”
“In the case of atrophic gastritis with hypochlorhydria and related malabsorption of dietary proteinbound vitamin B12, supplementation of vitamin B12 is recommended to ensure adequate vitamin B12 status.
“In contrast to vitamin B12 from natural foods, the absorption of crystalline vitamin B12 from preparations is not impaired in atrophic gastritis type B-related hypochlorhydria. However, investigations show that the use of dietary supplements or fortified foods reduces the prevalence of vitamin B12 deficiency in older people, but the risk of insufficient supply in general persists because of the dosage, which is often too low.”
For the assessment of the vitamin B12 status, a relevant functional parameter such as MMA should be combined with a status marker such as serum vitamin B12 or holo-TC.
A regular observation of the vitamin B12 status is recommended for (vegans, ovo-lacto vegeterians) and older people. For the assessment of the vitamin B12 status, a relevant functional parameter such as methylmalonic acid (MMA) should be combined with a status marker such as serum vitamin B12 or holo-TC.
Biomarkers of vitamin B12 status.
(A note: This section contains more information than was sent to our community member T. N. in our message. We added data to make the article that we are publishing on our websites more informative for the general community).
Serum or plasma vitamin B12 on its own is NOT sufficient to adequately assess vitamin B12 status.
Strohle, 2019:
“There are different biomarkers for assessing vitamin B12 status. These biomarkers include the two status parameters: vitamin B12 and holo-TC in serum or plasma and the functional parameters methylmalonic acid (MMA) and homocysteine in serum. However, none of these parameters is sufficient on their own to adequately assess vitamin B12 status. Furthermore, until now, no generally accepted cut-off values exist for any of the biomarkers.”
Biomarkers and proposed reference ranges of vitamin B12 status, a summary:
The following is derived from Strohle, 2019, and Lamers, 2011.
Plasma/serum B12: above 221 (pmol/L);
Plasma holo-transcobalamin (holo-TC): above 40 (pmol/L);
Plasma/serum methylmalonic acid (MMA) with normal creatinine: less than 210 (nmol/L) (or less than 270 nmol/L in Strohle, 2019);
Plasma homocysteine: less than 12 (umol/L, “micro mole per litre”).
What is methylmalonic acid (MMA)?
Methylmalonic acid (MMA) is a by-product of methylmalonyl-CoA. Methylmalonyl-CoA is a metabolite of the odd-chain fatty acid degradation pathway.
“Vitamin B-12 (cobalamin) serves as a cofactor in the folate-dependent homocysteine remethylation (Fig. 1) and in the formation of succinyl-CoA from methylmalonylCoA, a metabolite of the odd-chain fatty acid degradation pathway. Both pathways are sensitive to changes in vitamin B-12 status. Elevated plasma total homocysteine and methylmalonic acid (MMA) – a by-product of methylmalonyl-CoA – are sensitive functional biomarkers of vitamin B-12 status. Their specificity, however, is low due to several confounding factors and neither of the functional biomarkers can serve as sole parameter for reliable evaluation of vitamin B-12 status.”
“Figure 1 Schematic of one-carbon metabolism illustrating interdependent pathways of folate, vitamin B-12, and vitamin B-6.” Source: Lamers, 2011.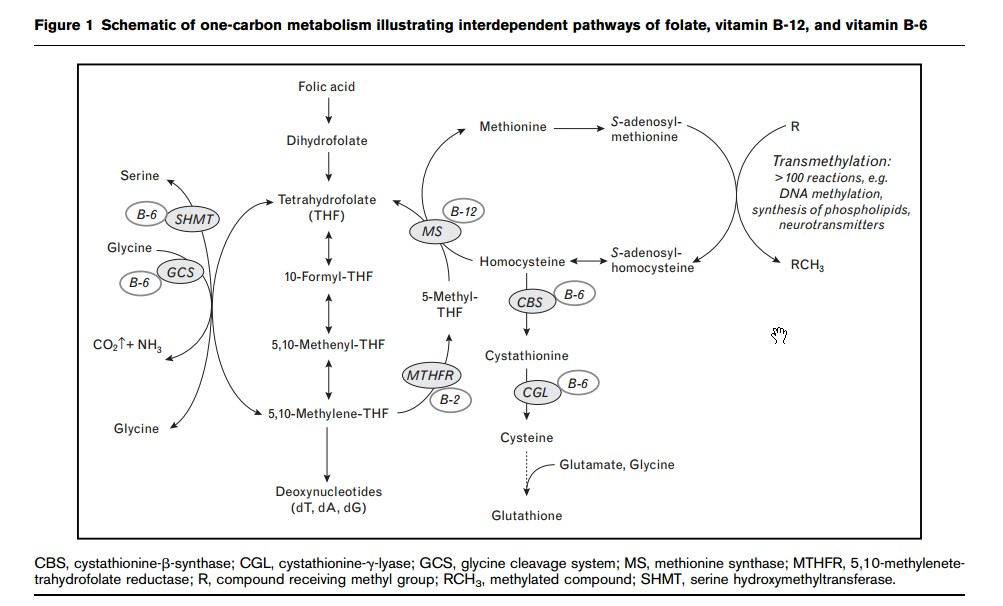 |
Strohle, 2019:
“Based on the data from the studies by Bor et al. and Pentieva et al. as well as on the target concentrations for total serum vitamin B12 (>221 pmol L −1 ), holo-TC (40 pmol L −1 ), MMA (<270 nmol L −1 ), and homocysteine (<12 µmol L −1 ), the estimated value for the vitamin B12intake is 4.0 µg d −1 for men and women within the age range of 19 and 65 years”
Clinical reference values and suggestive cut-offs for different levels of B-vitamin status. Source: Lamers, 2011.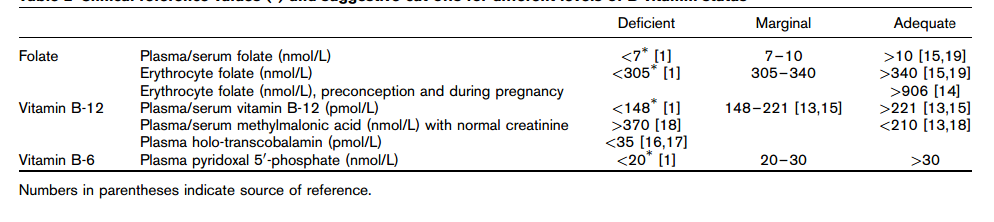 |
Criteria to derive the reference value of vitamin B12 intake in adults.
Strohle, 2019:
“As criteria to derive the reference value of vitamin B12 intake in adults, the serum concentrations of holo-TC (above 40 pmol L −1 ) and of the functional parameter MMA in the desirable range of less than 270 nmol L −1 are considered as the most important ones. These criteria are based on the results of two studies, in which the adequate vitamin B12 intake was determined using the serum concentrations of total vitamin B12and holo-TC as well as the functional parameters MMA and homocysteine. [13,14] In the cross-sectional study by Bor et al. [13] with subjects aged 18 to 50 years, an average serum holo-TC concentration of 65 pmol L −1 was reached with a daily median intake of 4.2 µg vitamin B12; higher intake levels were not associated with higher holo-TC concentrations. The serum concentration of vitamin B12 reached an average of 325 pmol L −1 . For the functional parameters MMA and homocysteine, average concentrations of 210 nmol L −1 and 8 µmol L −1 , respectively, were measured, [13] which indicate adequate vitamin B12supply. [28] The intake of morethan 7 µgd −1 during this study did not result in a further increase in the plasma vitamin B12 concentration. With an intake of 7 µg d −1 , the lowest serum concentrations of MMA and homocysteine were approximately 190 nmol L −1 and approximately 7 µmol L −1 , respectively.”
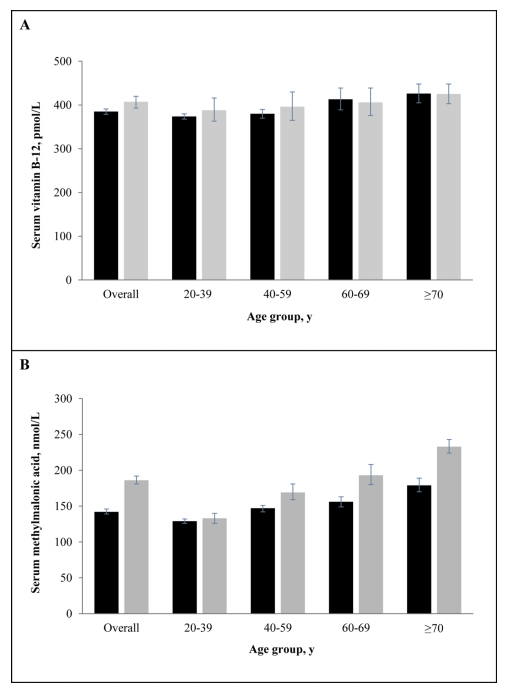
Additional information on vitamin B-12 and MMA: age-groups, supplements, renal function.
“Users of vitamin B-12 supplements had 40% higher serum vitamin B-12 concentrations, and approximately 5% lower MMA concentrations.”
“Impaired renal function was significantly associated with approximately 10–15% higher serum vitamin B-12 and approximately 50–70% higher MMA concentrations.”
Mineva et al., 2019 (1):
“Users of vitamin B-12 containing supplements had approximately 40% higher serum vitamin B-12 concentrations in both survey periods (statistically significant with and without controlling for other covariates), and approximately 5% lower MMA concentrations (statistically significant in 2013–2014 without and in both survey periods with controlling for other covariates).”
“Impaired renal function was significantly associated with approximately 10–15% higher serum vitamin B-12 and approximately 50–70% higher MMA concentrations in both survey periods, but for vitamin B-12 the association was no longer significant after controlling for other covariates.”
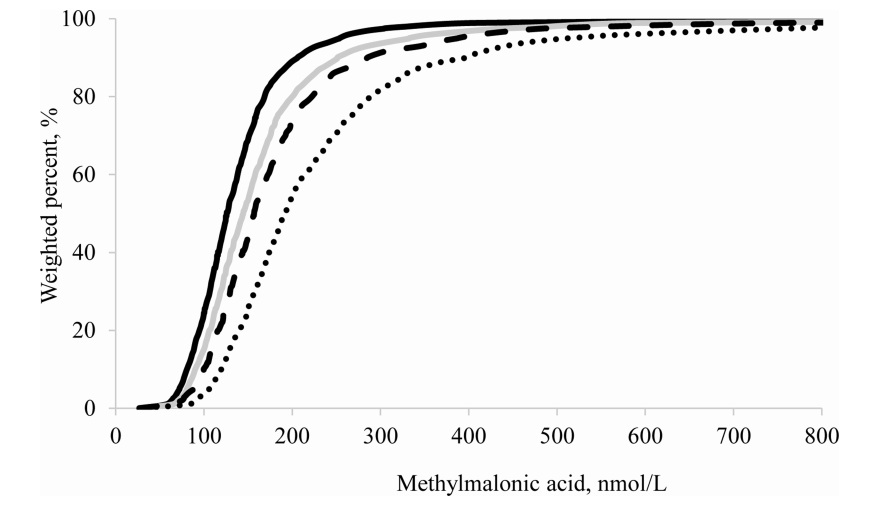
The need for age-specific reference intervals for vitamin B12 and MMA, especially in individuals aged above 70 years.
Mineva et al., 2019 (1):
”Vogiatzoglou et al.showed in a Norwegian population that the difference in MMA concentrations between middle-aged and elderly individuals was only partly explained by vitamin B-12 status and renal function [14], also suggesting the need for age-specific reference intervals.”
“Selected published reference intervals for serum or plasma methylmalonic acid.” Source: Mineva, 2019 (1).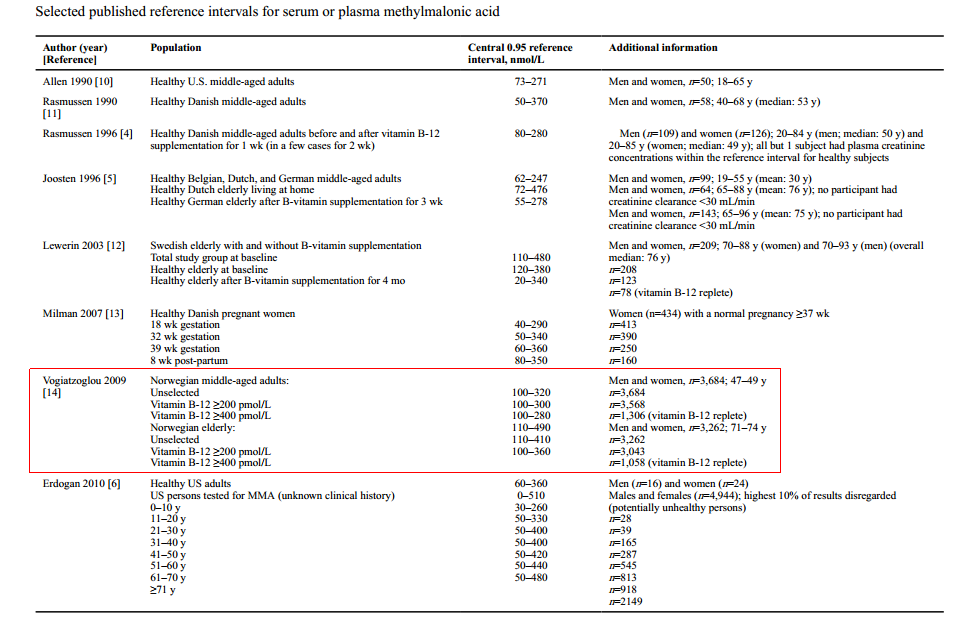 |
Age- and ethnicity-specific “health-associated” reference ranges and quintiles for vitamin B-12.
There is a more informative way to present the reference ranges than what was done by Mineva et al., 2019 (1), in the graphs and tables above.
George Cembrowski, a researcher, proposed a methodology and published a number of papers on the subject. Not only the mean or the 95% interval are presented, but also several additional quintiles.
The concentrations of vitamin B-12 tended to decline starting age 45-50 in as much as 50% of apparently healthy individuals (NHANES III, 1994). Vitamin B-12 is, therefore, a marker worth careful monitoring.
From the data presented by Cembrowski on one of his websites and reproduced below, we can see that the concentrations of vitamin B-12 tended to decline starting age 45-50 in as much as 50% of apparently healthy individuals. The conclusion is therefore that vitamin B-12 is a marker worth careful monitoring even in healthy.
Figure: Age- and ethnicity-specific “health-associated” reference ranges and quintiles for vitamin B-12. Source: Websites of George Cembrowski (accessed on January 10, 2022).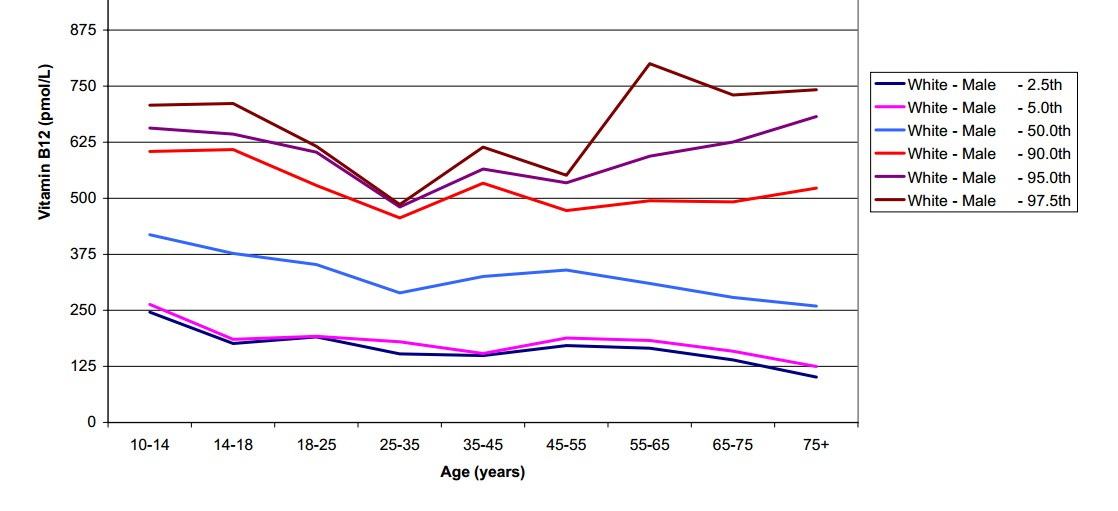 |
Several citations on Cembrowski’s methodology from his 2004 paper that covered other markers but gives a good idea of the approach used by the researcher.
Chembrovsky, 2004:
“Comprehensive, up-to-date “health-associated” reference interval studies of North American populations are uncommon. The third US National Health and Nutrition Examination Survey (NHANES III) was concluded in 1994 and yielded important reference interval data.”
“To determine health-associated reference intervals, we used the following exclusion criteria: pregnancy, breast feeding, obesity (body mass index [BMI] >40 and >35 for females and males, respectively), diastolic blood pressure >100 mm Hg, any smoking, any drinking of alcohol, recent treatment for anemia, creatinine level >2.5 mg/dL, glucose level >126 mg/dL, excessive thinness (BMI <8), recent surgery or hospitalization, or having antibodies to hepatitis viruses A, B, or C.”
Plasma total homocysteine as additional functional biomarker for vitamin B-12 status.
Homocysteine is only measured in plasma.
Lamers, 2011:
“Folate, vitamin B-12, and B-6 status can be assessed by direct measurement of their concentrations in plasma (or serum) and erythrocytes and by determination of functional biomarkers. All indicators discussed in this review can be measured in plasma or serum except for homocysteine that is only measured in plasma.”
Homocysteine is a sensitive but less specific indicator of vitamin B-12 status.
Lamers, 2011:
“Plasma total homocysteine underlies several confounding factors such as folate and vitamin B-6 status, renal function, age, and lifestyle factors. It is a sensitive but less specific indicator for vitamin B-12 status compared with MMA.”
Comparison of analytical methods for folate, vitamin B-12, and vitamin B-6 status assessment (“Table 1”). Source: Lamers, 2011.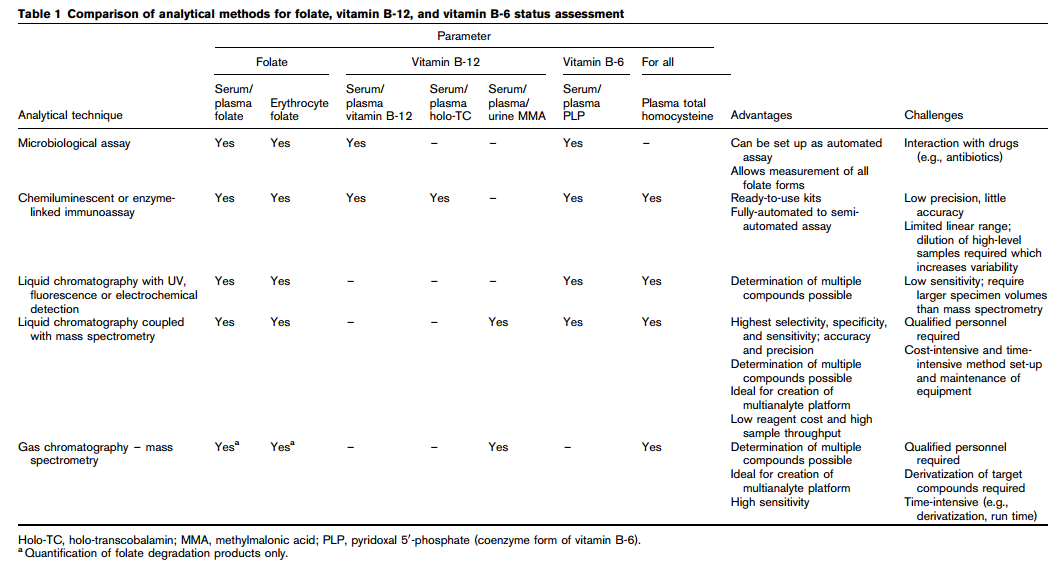 |
Questions (to T. N.) regarding vitamin B12 laboratory tests in the past.
Question (Q): Do you have data from your past laboratory tests on your serum/plasma vitamin B12? Were homocysteine, and other biomarkers of B12 status also assessed?
We are ending this message here. In our next communications, we will continue with the discussion and suggestions regarding (…) as well as other questions that came up in our exchanges.
Regards,
The team of The New Neander’s Medical.
Selected references:
1. Mineva EM, Sternberg MR, Zhang M, Aoki Y, Storandt R, Bailey RL, Pfeiffer CM. Age-specific reference ranges are needed to interpret serum methylmalonic acid concentrations in the US population. Am J Clin Nutr. 2019 Jul 1;110(1):158-168.